Estimation of Annual Risk of Tuberculosis Infection in Sri Lanka: an epidemiological approach for assessing the TB situation in the country.
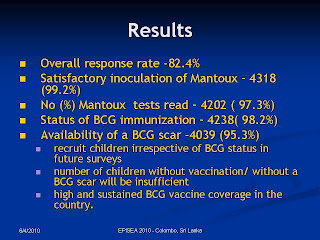
Methodology: A nation wide, school-based, cross sectional tuberculin survey was conducted to estimate the Annual Risk of Tuberculosis Infection (ARTI). The study sample comprised 5280 children aged 10 years irrespective of the BCG vaccination selected in a stratified, two stage cluster sampling technique. Of these, 4352 were administered tuberculin and reactions were read in 4202 within 72 hours according to a standardised protocol.
Results: The proportion immunized with BCG was 98% and 95% had a BCG scar. Frequency distribution of reactions demonstrated a not very distinct second mode corresponding to 15mm.Therefore; the mode of reaction sizes observed among 82 smear positive cases (20mm) was also studied. Both modes were used as cut off values for determining prevalence of TB by mirror image technique and ARTI as scenario one and two.
The national estimate of ARTI was 0.4% (95% CI- 0.2-0.7%) (Scenario I) and 0.12% ( 0.07-0.17%) (Scenario II). The corresponding values for urban, rural and estate strata were 1.4% (95CI- 0.8-2.1%), 0.2% (95CI- 0-0.6%) and 0.2 %( 95 CI- 0-0.7%) respectively, according to the scenario I. According to scenario II, ARTI estimates were 0.6% (95CI-0.08-1.2%) for urban, 0.12 %( 95CI- 0.07-0.2%) for rural, and 0.05% (95% CI- 0-0.2%) for estate sectors.
Conclusions: The national estimate of ARTI reflected a low risk of TB transmission. This estimate was lower than the same for many developing countries and higher than that for industrialised countries. ARTI in the urban stratum was higher than the national estimate.
The high ARTI in the urban sector calls for strengthening and intensifying TB control activities on sustained and long term basis. The low risk in other sectors does not allow complacency as reported incidence rate at present is less than the expected incidence of newly infected and re infected individuals .Sustained, committed , long term provision of quality anti tuberculosis service remains essential. A repeated tuberculin survey is recommended in 5-7 years for epidemiological trend analysis.